Candida auris: The new superbug on the block
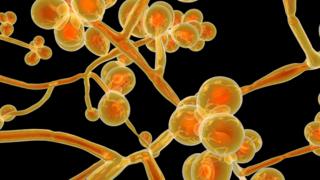 Image copyright Getty Images
Image copyright Getty Images The drug-resistant fungus, Candida auris, was only discovered 10 years ago, but is now one of the world’s most feared hospital microbes.
There have been outbreaks across the world, and new research shows higher temperatures may have led to an increase in infections.
The US Centers for Disease Control and Prevention (CDC) has called for better understanding of who is most vulnerable to reduce risk.
Here is everything you need to know about this new superbug.
What is Candida auris?
Candida auris (C. auris) is a yeast, a type of fungus, which can cause infections in humans.
It is related to the very common Candida albicans, which causes thrush.
It was first discovered in the ear canal of a Japanese patient in Tokyo Metropolitan Geriatric Hospital in 2009.
Most of the time, Candida yeasts live on our skin without causing problems, but they can cause infections if we are unwell or they get into the wrong place, like the bloodstream or lungs.
What sort of illness does it cause?
C. auris most frequently causes bloodstream infections, but can also infect the respiratory system, the central nervous system and internal organs, as well as the skin.
These infections are usually quite serious. Around the world, up to 60% of patients who get a C. auris infection have died.
The fungus is often resistant to the usual drugs, which makes infections difficult to treat.
Also, C. auris is often mistaken for a different infection, leading to the wrong treatment being given.
This means that the patient might be ill for longer or get worse.
“A number of UK hospitals have already experienced outbreaks requiring support from Public Health England,” said Dr Elaine Cloutman-Green, infection control practitioner and UCL clinical lecturer.
She added: “C. auris survives in hospital environments and so cleaning is key to control. Detection can be serious for both individual patients and for the hospital, as control can prove difficult.”
Dr Colin Brown, consultant medical microbiologist for Public Health England’s national infection service, said: “NHS hospitals that have experienced outbreaks of C. auris have not found it to be the cause of death in any patients.
“PHE is working closely with the NHS to provide expert support and advice on infection control measures to limit the spread of C. auris.”
Should I be worried about getting an infection?
It is unlikely that you will pick up a C. auris infection.
However, the risk is higher if you are in a hospital for a long time or if you are in a nursing home, and patients who are in intensive care are much more likely to get a C. auris infection.
The risk of picking up an infection is also higher if you have been on antibiotics a lot, because the drugs also destroy good bacteria that can stop C. auris getting in.
In the UK, about 60 patients have been infected by C. auris since 2013.
The Centers for Disease Control in the US has reported that globally, more and more countries are reporting cases of C. auris infections.
Most European countries have now reported some, with Greece being the last – in April this year.
Why is C. auris resistant to the usual drugs?
Resistance to the common antifungal drugs, like fluconazole, has been found in the majority of C. auris strains found in patients.
This means that these drugs do not work on C. auris. Because of this, less common antifungal drugs have been used to treat these infections, but C. auris has now developed resistance to these, too.
DNA evidence shows that the antifungal resistance genes in C. auris are very similar to those found in the very common C. albincans.
This suggests that the resistance genes have passed from one species to the other.
How can climate change be responsible for the high numbers of infections?
A study suggests that the reason C. auris infections have become so common may be because this species has been forced to live at higher temperatures because of climate change.
Most fungi prefer the cooler temperatures found in soil. But, as global temperatures have risen, C. auris has been forced to adapt to higher temperatures.
This may have made it easier for the fungus to thrive in the human body, which is warm at 36C to 37C.
What can be done to reduce the number of infections?
A better understanding of who is most at risk of contracting a C. auris infection is the first step to reducing the number of infections.
Healthcare professionals need to know that people who spend a long time in hospitals, nursing homes or are immunocompromised are at high risk.
Not all hospitals identify C. auris in the same way. They are sometimes mistaken for other fungal infections, like thrush, and the wrong treatment is given.
Improving diagnosis will help to identify patients with C. auris earlier, which will mean that the right treatment is given – preventing the spread of infection to other patients.
C. auris is very tough and can survive on surfaces for a long time.
It also cannot be killed using most common detergents and disinfectants.
Using the right cleaning chemicals is important to eliminate it from hospitals, especially if there is an outbreak.

